Big-model AI in drug design
Friday, April 28, 2023

The degree to which AI is profoundly transforming health and medicine might not be immediately apparent, even for close observers of artificial intelligence research. In the near term, interactions with medical staff are still largely analog, for example; but it is becoming quite clear, among people for whom the intersection of AI and human health is a passion, that all aspects of health and medicine are poised for change.
At the population level, data is driving massive changes in our understanding of wellness, illness, disease transmission, treatment efficacy, and more. Biobanks around the world are being mined by machine learning, computer vision, and natural language processing specialists, to realize as yet unthinkable or unattainable insights.
At the individual level, all of these insights are poised to drive rapid improvements in, and adoption of, personalized medicine. Researchers from around the globe are working towards a day when your individual biological makeup, informed by deep, nuanced insights from billions of your fellow humans, will be used to prescribe the optimal course of treatment for you at this moment in time.
So, the effect of AI on health is much more than just prescribing the right medication in the right dose. It promises the right medication, in the right dose, at the right time of day, and for the optimal duration based on what you eat, your genetic makeup, how much you sleep, how much stress you are under, and an infinite number of additional factors. Truly, if AI researchers in the human health space have their way, every imaginable factor will eventually be understood and accounted for, and your health will be fully optimized in the same way that high-performance engines or world-class instruments are tuned.
AI is driving improvements further upstream in fundamental research, drug development, and public health policy. Researchers and entrepreneurs in the space envision full-scale lab-on-a-chip technologies that completely remake our ability to understand biological systems; test the safety and efficacy of medicines; search for new ways to use existing medicines; and quite a bit else. The promise of AI in the health space is to shorten timelines from years to hours, reduce costs exponentially, and identify the most fruitful avenues for research years or decades earlier than might have previously been feasible.
To explore these topics and the state of AI in health more generally, an AI Quorum event was kicked off Monday, February 20, 2023, on the MBZUAI campus under the theme “Big Model AI in Drug Design.” The two-day workshop featured presentations from a range of speakers from public and private research institutions who are making unique, powerful contributions to the future of AI and health.
Pathways to personalized medicine
The workshop was opened by MBZUAI Adjunct Professor Eran Segal, who spoke about his work in the Human Phenotype Project. Segal explained that the Project works on the premise that the next leap in understanding human health and disease is going to come from modeling or measuring additional data about individuals such as environmental factors, physical activity, nutrition, and so on.
“I believe that such an approach is going to allow us to identify molecular signatures of disease before the disease appears, enabling us to predict disease ahead of time by identifying the trajectories that people are on,” said Professor Segal. “In some cases, it will also allow us to find the drivers of disease to identify therapeutic markers and this data will hopefully take us to personalized AI-based, and even remote, healthcare.”
One of the team’s efforts is in metagenomic sampling and associations with markers for obesity. The team conducts sequencing of human fecal samples and then records variations across samples and bacteria present – work that has established novel associations between body mass index (BMI) and the presence of certain gut bacteria, for example.
Another area that the team works on is the effects of medication on the human microbiome or gut environment. With large amounts of patient data, they were able to look at the effect that a whole range of medications has on patients and place the severity of effects along a useful spectrum that could help improve clinical advice and decision-making.
The ultimate goal of much of this work is to understand health trends with more nuance through the use of big data analysis across multiple axes, as well as to venture further into the personalized medicine space by giving individual patients scores that can be used to assess risks, opportunities for treatment, and more.
Watch Professor Segal’s full talk.
Pre-trained AI models for drug design
MBZUAI Professor of Machine Learning Le Song presented a talk titled, “Big Pre-trained AI Models for Drug Design.” Song outlined how, with drug discovery focused primarily on highly complex diseases such as cancer and other related conditions, the fundamental reason why developing drugs is hard is because the human body is such a complex, multi-scale dynamic system.
“In some sense, when something goes wrong in the human body, you can go from the organ level all the way down to the molecular level to find the places where the problem lies,” said Professor Song. “The core problem in drug design, target discovery, is to find the key node in this multi-scale network that is causing the problem and sometimes the key location or key molecule may not be just a single one, you might want to look at a combination of nodes in this complex network.”
He then spoke about his xTrimo system and delved into some of the specific ways that the model is trained on genetic data, and is able to make predictions in line with, or better than, systems such as AlphaFold, for example.
Watch his full talk here to learn more.
Leveraging biobanks
Following Professor Song, Aiden Doherty, Professor of Biomedical Informatics at Oxford University, discussed how he and his team have been conducting novel analysis of data from the UK Biobank. Doherty is interested in the kinds of insights that are hiding in biomarkers. How does sleep duration and quality correlate with mortality, for example?
Doherty’s team have taken pains to measure biomarkers of their own using wearable devices – data that they feed back into biobanks. And according to Doherty, the 10,000-step rule established in the 1970s is actually an agonizingly accurate goal for daily steps.
The team has made attempts to better understand sleep and its effects on mortality and a range of disease outcomes. Self-reported sleep studies are notoriously poor in the precision of their data collection. But the team has coupled wearable devices with deep learning techniques to harvest and analyze the massive amounts of data needed to glean real insights.
“What we need are more large-scale prospective biobanks. There are lots of amazing existing biobanks but mostly in Caucasian populations,” said Professor Doherty. “We just desperately need more large-scale, longitudinal biobanks in much more diverse populations across the world. And I think there is a real opportunity here in Abu Dhabi, where there is an amazing sequencing program, and if there is an opportunity to turn that into a biobank, that would be an incredible resource for the world, and really revolutionize what we can do in terms of genomic discovery and also in terms of wider research.”
The need for a medical culture change
MBZUAI President and University Professor Eric Xing played a key part in a panel that closed the AI Quorum and featured Le Song, Aidan Doherty, Uri Shalit, Omer Weissbrod, Alex Zhavoronkov, and Noa Dagan. Outlining how MBZUAI is building incubators and joint labs to enable a pipeline of tech transfer from the university to the business sector, he said: “The AI Quorum was developed to give researchers and entrepreneurs a chance to sit and discuss important topics outside the buzz and distraction of large conferences.”
In addition to answering questions from the audience, the panel engaged in a robust discussion on what will be the next approaches to drug development, with Professor Xing arguing that the current culture in medicine is an old-fashioned operational model bent on avoiding risk, but not suited to innovation.
“Why are we trying to design technology without a redesign? AI is best suited to revisit the pipeline of data collection, model design, and more to see what are the new dimensions that we might explore,” he said. “Do we need, for example, to follow a highly regulated and risk-averse approach? In health, I see a very big space where every stone could be overturned to find new solutions.”
More from the AI Quorum
Additional highlights of the event included Shai Shen-Orr (Technion) talking about his team’s work to address the explosion in the volume of academic publishing by employing natural language processing techniques to try to harvest insights from all of these published findings.
His Technion colleague Roy Kishony spoke about using AI to eliminate the need for broad spectrum antibiotic treatment based on a physician’s best guess. The team took sample, demographic, antibiotic use data, and moreover a 10-year period and fed this into a machine learning model for antibiotic resistance with the aim of developing personalized resistance predictions.
Orr Inbar, Co-Founder and CEO at QuantHealth discussed how the vast majority of drugs fail due to safety and efficacy issues and how in-silico medicine offers a powerful solution. This is particularly true when a condition is severe but rare and it is impossible to find populations large enough to do the kinds of research needed to generate understanding, and ultimately, therapies.
- university ,
- healthcare ,
- AI Quorum ,
- Drug design ,
Related
Intelligent, sovereign, explainable energy decisions: powered by open-source AI reasoning
As energy pressures mount, MBZUAI’s K2 Think platform offers a potential breakthrough in decision-making clarity.
- case study ,
- ADIPEC ,
- K2 Think ,
- IFM ,
- reasoning ,
- llm ,
- energy ,
- innovation ,
- research ,
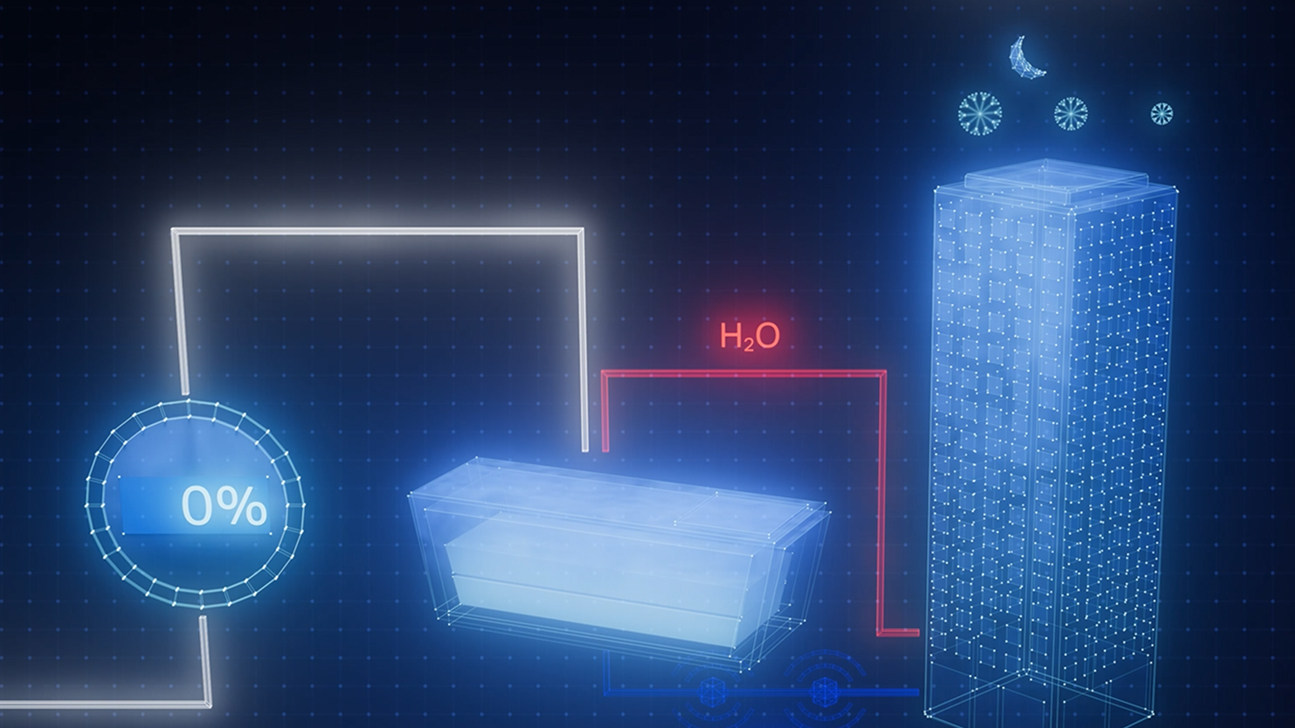
Cooling more people with fewer emissions: intelligent, efficient cooling with AI and ice batteries
MBZUAI's Martin Takáč is leading research to develop an AI-driven energy management system that optimizes the use.....
- energy ,
- cooling ,
- solar ,
- ADIPEC ,
- sustainability ,
- innovation ,
- research ,
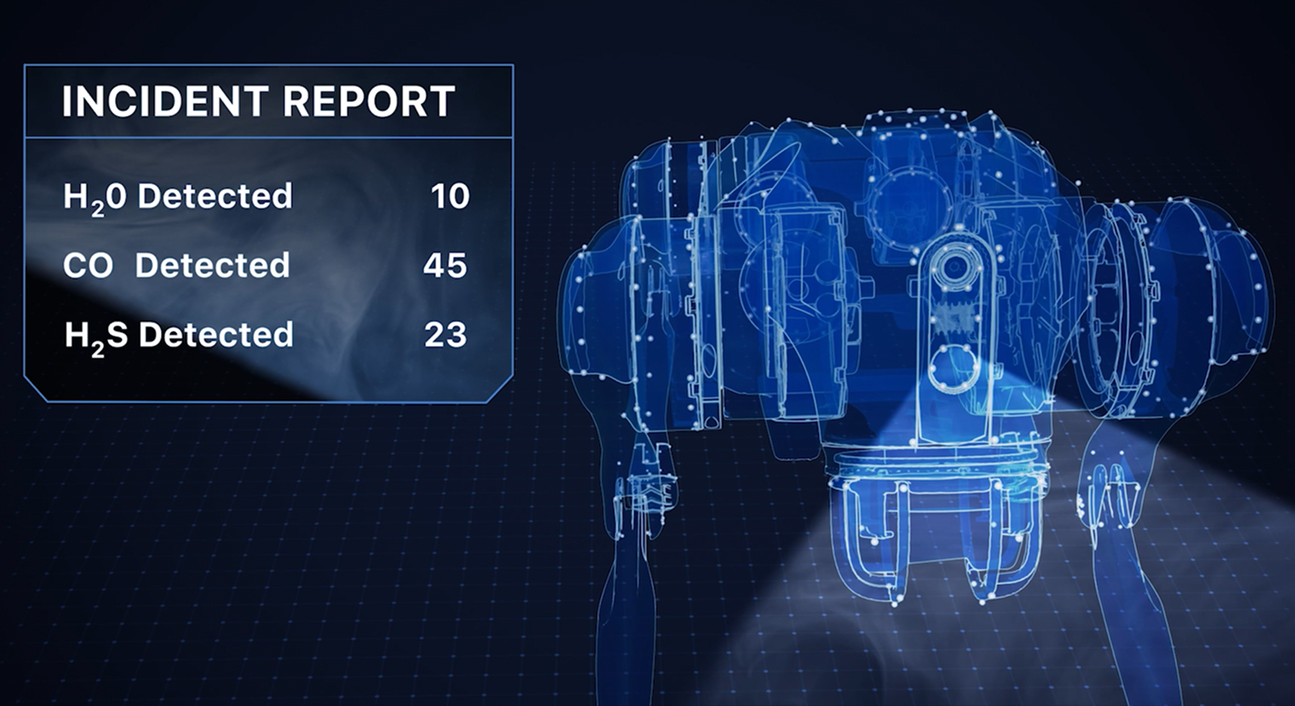
Faster, safer and smarter inspection: AI-powered robotics for industrial safety
MBZUAI's autonomous robotic system, LAIKA, is designed to enter and analyze complex industrial environments – reducing the.....
- research ,
- autonomous ,
- case study ,
- innovation ,
- infrastructure ,
- energy ,
- industry ,
- robotics ,